Hawaii Senior Living Guide: 5 Tips For Relating To Memory Loss
Hawaii Senior Living Checklist
4 Surprising Facts About Senior Living
Signs Your Loved One May Need More Help – What to Look for this Holiday Season
by Cara Clemmons, Director of Sales for The Plaza Assisted Living
With the holidays around the corner, many families are reconnecting with loved ones they may not have seen in some time. While 2020 has allowed for an endless amount of virtual visits, such as Zoom calls with Mom, there are key signs to look out for when visiting in person. Below are a few things to take notice of and consider, when determining if your loved one may be in need of more care than their current living situation provides.
- Is your loved one wearing the same clothes since the last time you spoke? Does your loved one look a bit disheveled or are they managing their grooming as they did before? Many adult children notice this as a sign that perhaps their loved one is not taking care of themselves as they used to. Sometimes this is due to activities of hygiene becoming challenging, as they age. Other times, this could be due to lack of routine, onset of dementia, or even geriatric depression.
- Has your loved one lost some weight? Weight loss can be a sign that your loved one needs more help. Older adults stop eating for a variety of reasons, and it is always a good idea to check in, to see what is happening, if you start to notice, they have shed a few pounds since last you saw each other. This can be for a variety of reasons including a lack of interest in food due to wakened sense of taste, side effects of medications, forgetting to eat, loss or weakened sense of taste, depression or even challenges securing groceries.
- Is your loved one repeating themselves often, seem a bit foggy or even aggressive? Forgetfulness and confusion happen to the best of us, and it is a normal part of the aging process. However, if you are noticing this more and more frequently with your loved one, this could be a sign of cognitive decline. Some experiencing cognitive decline can experience aggression as well, and this may be a big change in their behavior. If you are seeing these signs, it is always a good idea to check in with your loved one’s Primary Care physician, to monitor and even diagnose, if applicable.
- Are there any physical injuries you notice on your loved one, such as bumps, bruises, skin tears or burns? Are there any new visible damages to their vehicle or home? Physical injuries and visible property damage can sometimes be symptoms of larger safety concerns in your loved ones life. Many seniors may not remember a fall, but the physical injuries are a red flag, for you to investigate further.
- Does your loved one have any opportunities for socialization, or are they isolated? In the era of COVID-19, so many of the normal socialization opportunities that our Kupuna had to engage with their peers have faded away. Weekly choir practice has been canceled, church service has become virtual. Reach out to your loved one and see if they have opportunities for socialization and human connection. Socialization is not only good for cognitive health, but also good for the heart, as we are social beings who need interaction. This also helps combat loneliness, isolation and depression.
Cooking Corner Recipe: Shoyu Chicken

The Latest in Alzheimer’s and Brain Health Science
The Changing Face of Intimacy and Sexuality
Moving Evidence-Informed Assessment and Management of Behavioral Symptoms of Dementia into the Real World
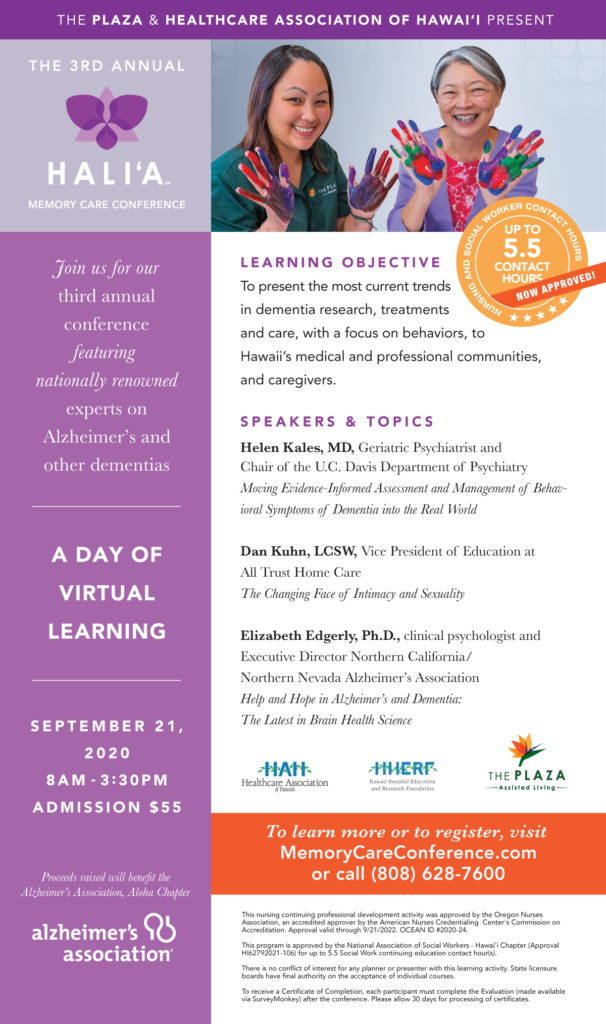
3rd Annual Hali’a Memory Care Conference – A Virtual Day of Learning